A dental abscess is a severe infection that occurs at the root of a tooth or between the tooth and the gum. If left untreated, it can lead to serious complications, including tooth loss, systemic infection, and even sepsis. In complex cases, treating and preventing dental abscesses requires a multi-faceted approach, which may involve infection control, root canal therapy, and additional advanced dental treatments. Understanding the causes, symptoms, and management options for dental abscesses is crucial for effective treatment and long-term oral health.
What is a Dental Abscess?
A dental abscess is a collection of pus caused by a bacterial infection, which can form at the root of a tooth (periapical abscess) or between the tooth and the gum (periodontal abscess). Abscesses occur when bacteria from untreated cavities, gum disease, or cracked teeth enter the tooth pulp or surrounding tissues, causing infection.
Common Causes of Dental Abscesses:
- Untreated cavities or decay that reach the tooth pulp
- Trauma or injury to a tooth, such as a crack or chip
- Periodontal disease (gum disease) leading to infection in the gum tissues
- Weakened enamel or poor dental restorations
Symptoms of Dental Abscesses
Recognizing the signs of a dental abscess early can help prevent more severe complications. Common symptoms include:
- Severe tooth pain, especially when chewing or applying pressure
- Swollen or painful gums
- Fever and a general sense of being unwell
- Bad taste or foul-smelling breath due to pus draining from the abscess
- Sensitivity to hot and cold
- Facial swelling near the abscessed tooth
Treatment Options for Dental Abscesses
1. Draining the Abscess
The first step in treating a dental abscess is to relieve the pus buildup by draining it. This helps reduce pain and prevents the infection from spreading. Drainage may be done through:
- Incision and drainage (surgically opening the abscess)
- Root canal therapy, if the abscess is caused by an infected tooth pulp
2. Antibiotics
Antibiotics are often prescribed to control infection, especially if the abscess has spread beyond the tooth. These may be used to treat:
- Localized infection around the abscess
- Systemic infections if the abscess has spread to the jaw, face, or even the bloodstream
However, antibiotics alone will not cure the abscess; they are often used in conjunction with other treatments like drainage or root canal therapy.
3. Root Canal Therapy
If the infection is deep in the tooth pulp (the innermost layer), root canal therapy is often necessary. This treatment involves:
- Removing the infected tissue
- Cleaning the root canal to eliminate bacteria
- Sealing the canal to prevent further infection
Root canal therapy can save the tooth, remove the infection, and prevent the need for extraction.
4. Tooth Extraction
In severe cases where the tooth is beyond repair or if there is extensive damage, extraction may be necessary to prevent the infection from spreading further. After the tooth is removed, the area can be cleaned and treated to ensure proper healing.
Preventing Dental Abscesses in Complex Cases
Prevention is the key to avoiding dental abscesses, especially for patients with complicated oral health needs or those who have experienced abscesses in the past. Here are some strategies to reduce the risk:
1. Good Oral Hygiene Practices
Maintaining excellent oral hygiene helps reduce plaque and bacteria buildup, preventing cavities and gum disease that can lead to abscesses. This includes:
- Brushing teeth at least twice a day with fluoride toothpaste
- Flossing daily to remove debris from between the teeth and gums
- Using an antimicrobial mouthwash to control bacteria
2. Regular Dental Checkups
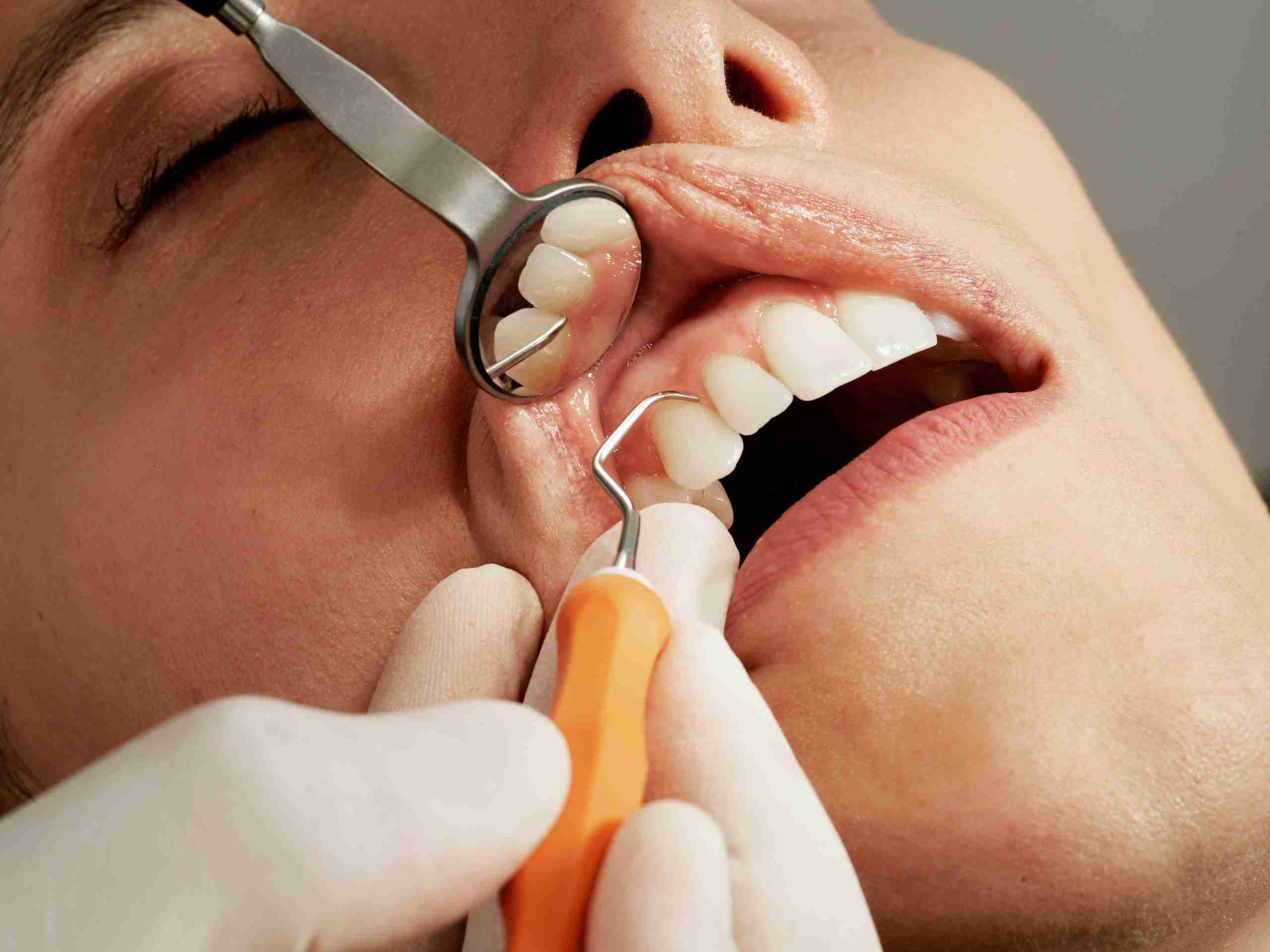
Routine dental exams allow the dentist to catch and treat problems early. Regular cleanings and professional checkups can detect cavities, gum disease, or other issues that might lead to abscesses.
3. Treating Cavities Early
Addressing cavities in their early stages can prevent the infection from reaching the tooth pulp and causing an abscess. This includes filling cavities as soon as they are detected.
4. Addressing Periodontal Disease
Patients with gum disease or periodontitis are at higher risk for developing dental abscesses. Timely intervention to treat gum disease, such as scaling and root planing, can prevent bacterial infection from reaching the tooth roots.
5. Dietary Adjustments
A balanced diet that promotes tooth enamel health can reduce the risk of tooth decay and infection. Limiting sugary and acidic foods can help prevent cavities and the bacterial overgrowth that causes abscesses.
6. Protective Dental Appliances
For patients with a high risk of trauma, such as athletes or those who grind their teeth at night (bruxism), wearing mouthguards or nightguards can protect the teeth from damage and reduce the risk of developing an abscess from cracked or chipped teeth.
When to Seek Immediate Dental Care
A dental abscess is a serious condition that can worsen rapidly. If you experience any of the following, it’s essential to seek dental care immediately:
- Severe pain that doesn’t subside
- Swelling of the face or jaw
- Fever or chills
- Difficulty swallowing or breathing
- A foul-tasting drainage or pus in the mouth
Delaying treatment could lead to more severe complications, including sepsis, bone damage, or tooth loss.
Treating and preventing dental abscesses in complex cases requires prompt diagnosis and a comprehensive approach, combining techniques like root canal therapy, antibiotics, and infection control. Regular dental visits, excellent oral hygiene, and early intervention are essential in preventing abscesses and preserving long-term oral health. By understanding the causes and symptoms of dental abscesses, patients can take steps to protect themselves from this painful and potentially dangerous condition.
Leave a Reply